On this page
- Fee-for-service and alternative payment approaches
- Outcome payments can be effective when well designed
- ‘Enrolment’ approaches
- ‘Blended’ payment approaches
- Finding 2: The fee-for-service payment approach rewards NDIS providers for the volume of supports they deliver, rather than for supporting participants to achieve outcomes
Currently providers are paid based on the services they provide, rather the benefits of those services to participants. Providers should be rewarded for helping to achieve participant goals. This would benefit the providers who provide high-quality services, and it increases the focus for Government, the NDIS and providers on building the long-term capabilities of participants.
While price caps and controls are important, how we pay providers also matters. The interplay between pricing and payment approaches has a critical role in what supports are supplied to the market and the outcomes achieved for participants.
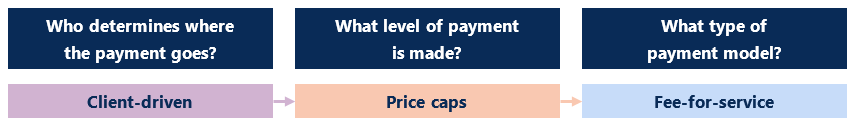
The pricing and payment approach used in the NDIS is centred on a market-based model, which includes fee-for-service payments and capped prices for supports (Figure 12).
Fee-for-service and alternative payment approaches
The NDIS operates largely through a fee-for-service payment model. Providers are paid for each unit of service delivered, rather than the benefits of those services to participants.
This approach is easy to administer and understand. However, it rewards providers for the volume of service they deliver, regardless of the ‘value’ for participants. Providers have a financial incentive to provide more and more services and/or increase staff ratios regardless of the benefit.
There could be benefits from shifting away from the one-size-fits-all, fee-for-service payment approach in the NDIS.
While fee-for-service is a common way to pay providers of social services, there are alternative payment approaches, which are used across different social markets (Figure 13).[62] Each payment approach has advantages and disadvantages and rewards different sorts of behaviour by providers.
For example, activity-based payments are used to pay public hospital and aged care providers under the Australian National Aged Care Classification (AN-ACC) (introduced in October 2022). While a form of fee-for-service, activity-based payments cover a bundle of services provided rather than each individual service. For example, for public hospitals this may include the accommodation, surgery, pathology, nursing and medicines costs for an episode of care. When compared to a fee-for-service payment, activity-based payments strengthen incentives for providers to reduce costs. Activity-based funding, however, can be more complex to administer and requires more detailed data.
Beyond variations on fee-for-service, introducing different payment approaches could help ensure the service offering of providers better reflect the nature of supports. For example, enrolment payments could be used where support needs are more predictable and less episodic in nature.
Outcome payments can be effective when well designed
Paying for outcomes in the NDIS, when well designed, could strengthen incentives to deliver evidence-based and timely services.
The NDIA’s 2018 Independent Pricing Review, conducted by McKinsey & Company, suggested that over the long term the development of a competitive marketplace should enable changes to the scheme’s current model of using price caps and fee for service. The report recommended trialling outcomes-based pricing in the NDIS.
Firstly, the NDIA should conduct a trial of outcomes-based pricing. This is an appealing alternative to input-based pricing as it encourages providers to maximise outcomes, rather than the volume of services provided. However, it is significantly more complex and requires strong baseline data and measurement systems. A trial would provide valuable learnings on how this approach might be implemented in some supports.
Outcome payments have been used in other social services.
For example, employment service providers are paid in part for supporting people to achieve employment outcomes. Participants in mainstream and Disability Employment Services can also choose their provider on the basis of the provider’s past outcomes or performance via a ‘star rating’. In addition, under the previous jobactive scheme, every 18 months, higher performing employment providers were allocated a larger market share, while poorer performing providers lost market share.
Experience in other social services has shown that providers can be responsive to outcome payments, which can drive benefits for participants.
The New South Wales Family Preservation Service has highlighted some of the benefits of payment-by-result. The program supports children at risk of entering out-of-home-care by proving a range of supports including therapy, social work and personal care services. A 2020 independent evaluation of the program found the payment-by-results approach reduced entry to acute settings. The evaluation also found material cost savings with higher uptake of preventative actions. Clients with high and complex needs were found to benefit most.[65]
However, it can be difficult to link outcomes to providers’ performance. Providers may not want to supply the market where too much of the payment is at risk. Providers also require the necessary scope to drive positive outcomes for participants. To affect an outcome, providers may need to be able to offer a ‘bundle’ or ‘wrap around’ supports.
Back to top‘Enrolment’ approaches
Approaches where participants ‘enrol’ with a provider for a period can strengthen the focus on providers’ relationship with participants and encourage them to invest in participants’ capability (Figure 14). Enrolment approaches also have the potential to stabilise the demand profile for providers. In turn, this may assist providers to shift away from a more casual workforce.
Careful design would be required to mitigate the risk of poor outcomes under enrolment approaches. This includes careful monitoring and feedback loops to address the risk of provider’s limiting access to services required to meet the needs of participant, or under servicing.
Providers may also ‘cherry-pick’ participants if enrolment payments are not risk-weighted for the additional costs of supporting participants with complex support needs. Importantly, any adjustment for risk needs to be based on factors that cannot be manipulated by the service providers. Otherwise it is possible for providers to focus more on capturing the payments than improving outcomes for participants.
Back to top‘Blended’ payment approaches
Paying providers a ‘blended’ payment’ – that is, based on a mix of payment approaches – could help balance the advantages and disadvantages of particular payment approaches and better align incentives between participants, providers, and governments.
Well-designed blended payment approaches could put a greater focus on participant outcomes without relying wholly on a pure outcome payment. For example, enrolment arrangements, when blended with outcome payments, can incentivise providers to reduce costs through providing fewer, or less costly, supports and investing in cost-effective preventive and early intervention services.
Blended payment models would allow participants to pay providers in another way instead of only fee-for-service, for example paying more for a provider who can demonstrate high quality service delivery, or paying a provider for meeting a participant’s needs for trust, stability, and relationships over a period of time instead of service-by-service.
Any such approaches would benefit from an outcomes framework that measures whether providers are delivering positive outcomes for participants. This would take considerable time to ‘get right’.
